Click here to visit the publication at the Australian Government website.
Background:
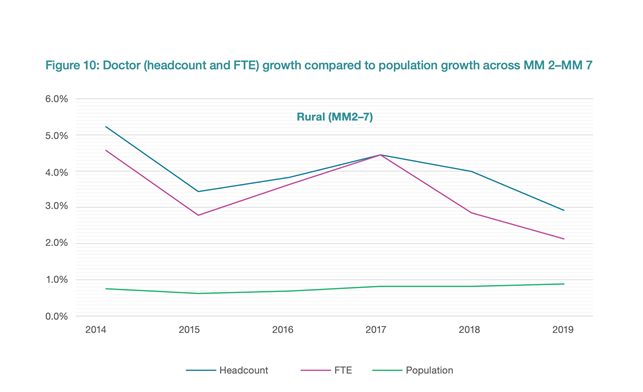
Australia has not been able to sustain a medical workforce which was distributed in the same proportions as the Australian population.
Around seven million people, or 29% of Australia’s population, live in rural and remote areas.
Yet the distribution of medical graduates is vastly different[1]:
Quotes from the National Medical Workforce Strategy, endorsed by Australian Health Ministers in December 2021:
The medical workforce has a profound impact on the quality, accessibility, effectiveness and sustainability of the health system. However, inequality of access to health services remains a key issue for Australian communities. To achieve maximum benefit to the community, the medical workforce must be geographically well distributed and have the appropriate mix of medical specialties in each location.
Investment in metropolitan tertiary centres provides high-quality services but has created metro-centric training systems… During consultations on the Strategy, selection of trainees was criticised for its focus on academic skills rather than the broad range of skills needed for the specific specialty.
The National Medical Workforce Strategy notes the way this has discouraged medical specialist training in non-Metropolitan centres and proposed a broad suite of measures aimed at correcting this:
The intent is to increase training opportunities in rural locations that support trainees to complete the majority of their training in a rural location… As regional and rural registrars, they should have preferential access and support for any training required in metropolitan hospitals. This enables doctors to settle in a community when they are typically forming partnerships, building a family and a home.
A number of specialist medical colleges are developing pathways to provide more rural training. One example of this is the Royal Australasian College of Surgeons Rural Committee and its development of a Rural Health Equity Strategic Action Plan, which outlines its rural health strategies Represent for Rural, Select for Rural, Train for Rural, Retain for Rural and Collaborate for Rural.
The Regional Training Hubs are designed to facilitate this ‘end-to-end’ approach. They are based in Universities with substantial rural campuses and clinical schools. Their aim is to work across the continuum of medical training to help Universities, State Health Departments and specialist training colleges to build the resources and support systems to:
- Recruit more students from rural/regional areas into medical schools;
- Establish more medical school places in rural/regional locations;
- Have more internship and junior doctor training based in rural/regional locations, and
- Establish post-graduate specialist (including Rural Generalist) training programs which are predominantly based in non-Metropolitan centres.
The current Regional Training Hubs are:
The RMSA supports this policy and is eager to work with all parties including the Regional Training Hubs to achieve the aim of steady but sustained re-alignment of the Australian Medical workforce to the distribution and make-up of the Australian people.
_______________
1MM refers to the Modified Monash Model. The Modified Monash Model (MM) defines whether a location is a city, rural, remote or very remote. The model measures remoteness and population size on a scale of MM category MM 1 to MM 7, with M1 being major metropolitan areas and M7 very remote communities (eg Longreach, Coober Pedy)
